אמנות הטיפול התרופתי בכאב בחולה האונקולוגי המבוגר - נייר עמדה - Pharmacological pain treatment in adults oncology
|
| |
|---|---|
| אמנות הטיפול התרופתי בכאב בחולה האונקולוגי המבוגר - Pharmacological pain treatment in adults oncology | |
| תחום | רפואה פליאטיבית, פרמקולוגיה קלינית |

| |
| האיגוד המפרסם | איגודים משתתפים |
| קישור | באתר הר"י |
| תאריך פרסום | 2019 |
| יוצר הערך | העורכים |
| ניירות עמדה מתפרסמים ככלי עזר לרופא/ה ואינם באים במקום שיקול דעתו/ה בכל מצב נתון. כל הכתוב בלשון זכר מתייחס לשני המגדרים. | |
לערכים נוספים הקשורים לנושא זה, ראו את דף הפירושים – כאב במחלות ממאירות
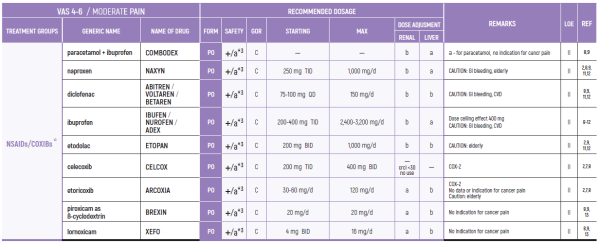
LEVELS OF EVIDENCE & GRADES OF RECOMMENDATION
(Adapted from the Infectious Diseases Society of America-United States Public Health Service Grading System)
LEVELS OF EVIDENCE (LOE)
- I - Evidence from at least one large randomised, controlled trial of good methodological quality (low potential for bias) or meta-analyses of well-conducted randomised trials without heterogeneity
II - Small randomised trials or large randomised trials with a suspicion of bias (lower methodological quality) or meta-analyses of* such trials or of trials demonstrated heterogeneity
- III - Prospective cohort studies
- IV - Retrospective cohort studies or case-control studies
- V - Studies without control group, case reports, expert opinions
GRADES OF RECOMMENDATION (GOR)
- A - Strong evidence for efficacy with a substantial clinical benefit, strongly recommended
- B - Strong or moderate evidence for efficacy but with a limited clinical benefit, generally recommended
C - Insufficient evidence for efficacy or benefit does not outweigh the risk or the disadvantages (adverse events, costs, . . .),* optional
- D - Moderate evidence against efficacy or for adverse outcome, generally not recommended
- E - Strong evidence against efficacy or for adverse outcome, never recommended
מקור:
(*) Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149–iv174
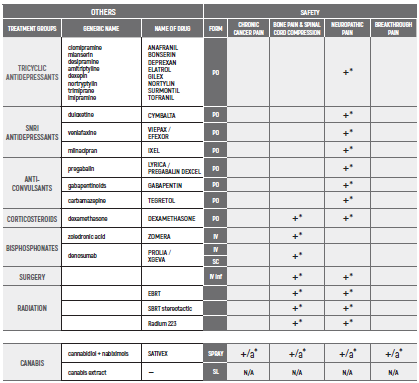
CHRONIC PAIN/ד"ר אורה רוזנגרטן
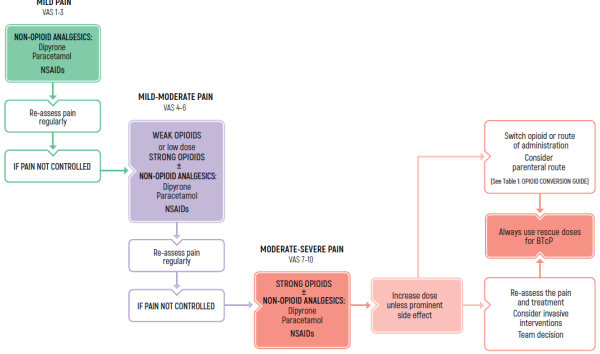
TREATMENT OF CHRONIC PAIN
- Use around the clock-long acting medications
- Allow rescue medications
(*) Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149–iv174.
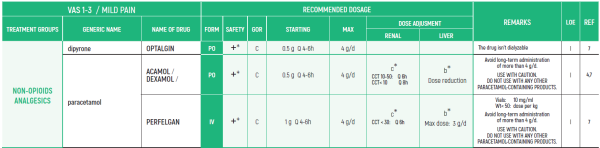
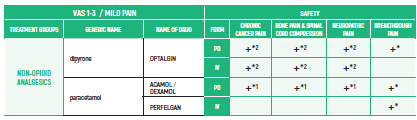
ADULTS/Chronic Cancer Pain
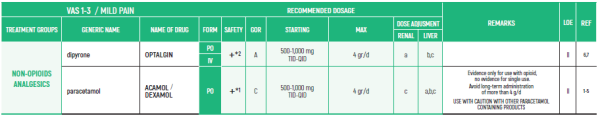
NON-OPIOIDS ANALGESICS:
- PARACETAMOL: Avoid long-term administration of more than 4 g/d (gram/day). Avoid when patient is ingesting limited food or consumes long-term ethanol
- DIPYRONE/METAMIZOLE: Agranulocytosis has been described with varying relative risks in different populations. Patients should be advised to seek for medical care if signs of infection
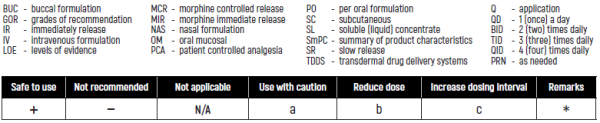
- BUC - buccal formulation
- GOR - grades of recommendation
- IR - immediately release
- IV - intravenous formulation
- LOE - levels of evidence
- MCR - morphine controlled release
- MIR - morphine immediate release
- NAS - nasal formulation
- OM - oral mucosal
- PCA - patient controlled analgesia
- PO - per oral formulation
- SC - subcutaneous
- SL - soluble (liquid) concentrate
- SmPC - summary of product characteristics
- SR - slow release
- TDDS - transdermal drug delivery systems
- Q - application
- QD - 1 (once)a day
- BID - 2 (two) times daily
- TID - 3 (three) times daily
- QID - 4 (four) times daily
- PRN - as needed
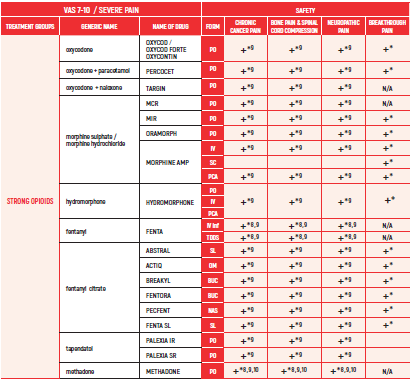
ADULTS/Chronic Cancer Pain
LIMITED USE FOR SHORT PERIODS ONLY RESPONDING PATIENTS: RE EVALUATE FOR LONG TERM USE RISK FACTORS.
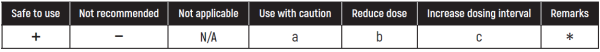
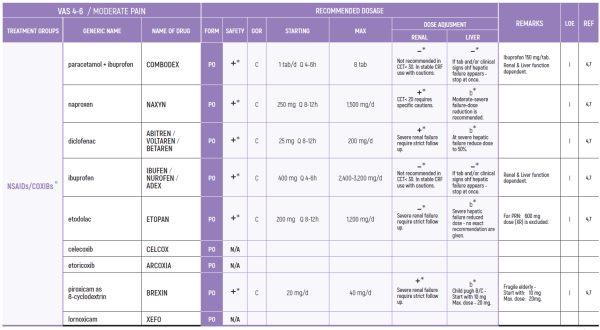
NSAIDs:
3. Prolonged use not advised due to concern of side effects such as hypertension, edema, CVD (Cardiovascular Disease), GI bleeding, renal toxicity and bleeding diathesis weak opioids (8)
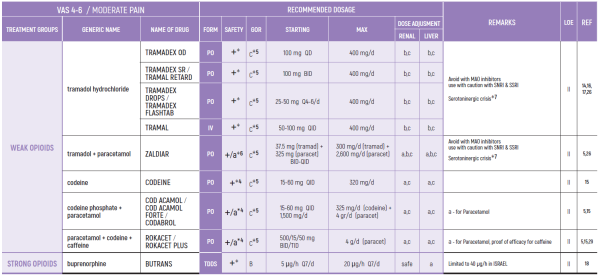
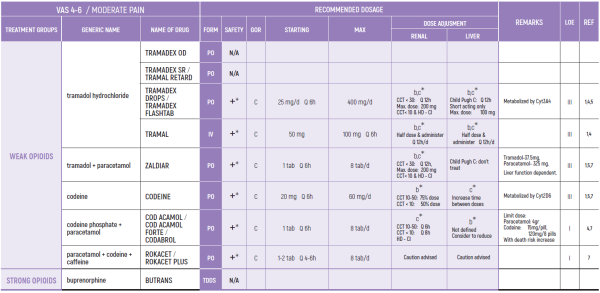
WEAK OPIOIDS:
2. Ceiling effect may reduce efficacy and induce side effects (26)
3. Compared to low dose strong opioids - better and faster effect by strong opioids (14)
4. Use with caution with other paracetamol containing products
5. Tramadol may cause serotoninergic crisis, mostly in elderly, although uncommon (26)
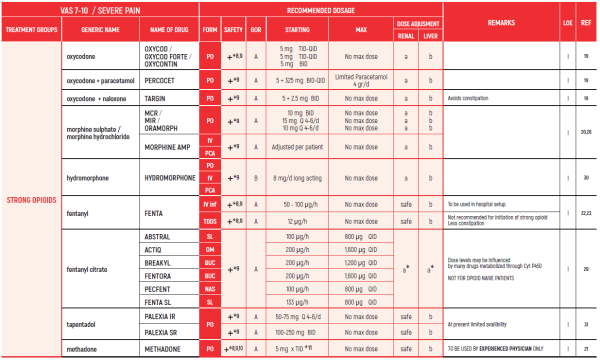
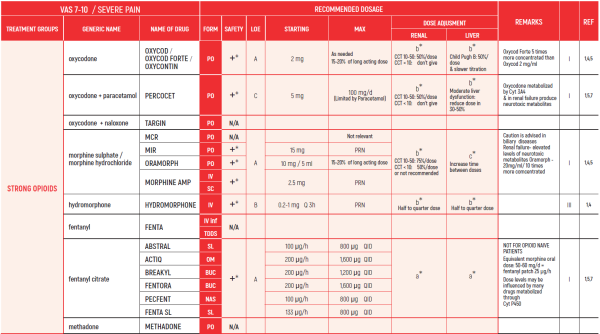
STRONG OPIOIDS:
6. Beware in elderly - may develop confusion
7. Discontinuation should be gradual to avoid withdrawal symptoms
10. Methadone is equivalent to morphine in terms of efficacy but needs careful titration. Half-life may differ between people - careful titration needed. Advised to be used by experts only
11. Methadone starting dose depends on dose of opioid used previously. Equivalence doses of methadone differ at low and high doses of morphine
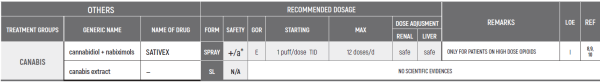
SATIVEX is indicated as adjunctive treatment for the symptomatic relief of neuropathic pain in multiple sclerosis in adults.
SATIVEX may be useful as adjunctive analgesic treatment in adult patients with advanced cancer who experience moderate to severe pain during the highest tolerated dose of strong opioid therapy for persistent background pain.
The indications in the Ministry of Health’s “Procedure 106” are:
2.3.0.0. For patients during treatment with chemotherapy and up to six months after its completion to relieve nausea, vomiting, or pain related to treatment (even without exhaustion of conventional treatments for relief of nausea, etc.). In cases where the attending physician believes cannabis treatment should be continued after half a year- he will specify the reasons for the continuation of the treatment and for what period he believes the treatment should be continued
22.3.0.3 To relieve pain from a cancerous source at the metastatic stage and after exhausting conventional treatment options
- ביבליוגרפיה
- Leslie A. Shimp, Pharm.D., Safety Issues in the Pharmacologic Management of Chronic Pain in the Elderly. Pharmacotherapy 1998; 18(6):1313-22
- https://www.drugs.com/dosage
- Cooper TE, Fisher E, Anderson B, Wilkinson NMR, Williams DG, Eccleston C, Paracetamol (acetaminophen) for chronic non-cancer pain in children and adolescents (Review), Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No.: CD012539
- Wiffen PJ, Derry S, Moore RA, McNicol ED, Bell RF, Carr DB, McIntyre M, Wee B. Oral paracetamol (acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No.: CD012637
- Israel JF, Parker G. Llack of benefit from paracetamol in palliative cancer patients reguiriing high doses of opioids: a randomised double blind placebo controlled trial, J Pain and Symptom Management, March 2010; 39(3)
- Gaertner J, Stamer UM, Remi C, Voltz R, Bausewein C. Metamizole/dipyrone for the relief of cancer pain: A systematic review and evidence-based recommendations for clinical practice. Palliat Med. 2017 Jan; 31 (1): 26-34
- Levy M, Zylber-Katz E, Rosenkranz B. Clinical Pharmacokinetics of Dipyrone and its Metabolites, Clinical Pharmacokinetics. March 1995; 28(3): 216-234
- Mercandante S, Giarratano A. The long and winding road of non steroidal antinflammatory drugs and paracetamol in cancer pain management: A critical review Critical Reviews in Oncology/Hematology, August 2013; 87(2): 140-5
- Derry S, Wiffen PJ, Moore RA, McNicol ED, Bell RF, Carr DB, McIntyre M, Wee B. Oral nonsteroidal anti-inflammatory drugs (NSAIDs) for cancer pain in adults. Cochrane Database of Systematic Reviews 2017, Issue 7.
- Moore RA, Derry S, Wiffen PJ, Straube S, Aldington DJ. Overview review: Comparative efficacy of oral ibuprofen and paracetamol (acetaminophen) across acute and chronic pain conditions. Eur J Pain (2015);19:1213-23
- Ventafridda V, De Conno F, Panerai AE, Maresca V, Monza GC, Ripamonti C. Non-steroidal anti-inflammatory drugs as the first step in cancer pain therapy: double-blind, within-patient study comparing nine drugs.J Int Med Res. (Jan-Feb 1990); 18(1): 21-9
- Ewan D McNicol Scott Strassel sLeonidas Goudas Joseph Lau Daniel B Carr: NSAIDS or paracetamol, alone or combined with opioids, for cancer pain, Cochrane Systematic Review: 20 April 2005
- Yalcin S, Altundag K, Asil M, Tekuseman G. Sublingual Piroxicam for cancer pain . Med Oncol (Jul 1998); 15(2): 137-9
- Bandieri E, Romero M, Ripamonti Cl, Artioli F, Sichetti D, Fanizza C, Santini D, Cavanna L, Melotti B, Conte PF, Roila F, Cascinu S, Bruera E, Tognoni G, Luppi M. Randomized Trial of Low-Dose Morphine Versus Weak Opioids in Moderate Cancer Pain. J Clin Oncol. (Feb 2016) 10; 34(5): 436-42
- Straube C, Derry S, Jackson KO, Wiffen PJ, Bell RF, Strassels S, Straube S. Codeine, alone and with paracetamol (acetaminophen), for cancer pain.Cochrane Database of Systematic Reviews 2014, Issue 9.
- Eisenberg E, Berkey CS, Carr DB, Mosteller F, Chalmers TC. Efficacy and safety of nonsteroidal antiinflammatory drugs for cancer pain: a meta-analysis. J Clin Oncol. (Dec 1994); 12)12): 2756-65
- Wiffen PJ, Derry S, Moore RA. ramadol with or without paracetamol (acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 5
- Schmidt-Hansen M, Bromham N, Taubert M, Arnold S, Hilgart JSSchmidt-Hansen M, Bromham N, Taubert M, Arnold S, Hilgart JS. Buprenorphine for treating cancer pain .Cochrane Database of Systematic Reviews 2015, Issue 3
- Schmidt-Hansen M, Bennett Ml, Arnold S, Bromham N, Hilgart JS., Oxycodone for cancer-related pain. ,Cochrane Database of Systematic Reviews 2017, Issue 8.
- Wiffen PJ, Wee B, Moore RA., Oral morphine for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 4.
- Nicholson AB, Watson GR, Derry S, Wiffen PJ. Methadone for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 2
- Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain. Cochrane Database of Systematic Reviews 2013, Issue 10
- Corli 0, Floriani I, Roberto A, Montanari M, Galli F, Greco MT, Caraceni A, Kaasa S, Dragani TA, Azzarell0 G, Luzzani M, Cavanna L, Bandieri E, Gamucci T, Lipari G, Di Gregorio R, Valenti D, Reale C, Pavesi L, lorno V, Crispino C, Pacchioni M, ApoIone G; CERP STUDY OF PAIN GROUP: Are strong opioids egually effective and safe in the treatment of chronic cancer pain? A multicenter randomized phase IV 'real life' trial on the variability of response to opioids. Ann Oncol. (Jun 2016); 27(6): 1107-15
- Sande TA, Laird BJ, Fallon MT, The use of opioids in cancer patients with renal impairment-a systematic review, Support Care Cancer. (Feb 2017); 25(2): 661-75
- King S, Forbes K, Hanks GW, Ferro GJ, Chambers EJ. A systematic review of the use of opioid medication for those with moderate to severe cancer pain and renal impairment: a European Palliative Care Research Collaborative opioid guidelines project. Palliat Med.(Jul 2011); 25(5): 525-52
- Fallon M, Giusti R, Aie 11 i F, Hoskin R Rolke R, Sharma M, Ripamonti Cl; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149-iv174.
- Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT. Results of a Double- Blind, Randomized, Placebo-Controlled Study of Nabiximols Oromucosal Spray as an Adjunctive Therapy in Advanced Cancer Patients with Chronic Uncontrolled Pain, J Pain Symptom Manage. (Feb 2018): 55(2): 179-88
- Jandhyala R, Fullarton JR & Bennett Ml. Efficacy of Rapid-Onset Oral Fentanyl Formulations vs. Oral Morphine for Cancer- Related Breakthrough Pain: A Meta-Analysis of Comparative Trials. J Pain Symptom Management 2013 Oct; 46 (4): 573-80
- Mitchell A, McCrea P, Inglis K, Porter G. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine (Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012 Nov; 19(12):3792-800
- Bao YJ, Hou W, Kong XY, Yang L, Xia J, Hua BJ, Knaggs R. Hydromorphone for cancer pain. Cochrane Database Syst Rev. 2016 Oct 11;10
- Mercadante S. Opioid titration in cancer pain: a critical review. Eur J Pain. 2007 Nov;11(8):823-30
- Fallon MT, Albert Lux E, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Lichtman AH & Kornyeyeva E. Sativex oromucosal spray as adjunctive therapy in advanced cancer patients with chronic pain unalleviated by optimized opioid therapy: two double-blind, randomized, placebo-controlled phase 3 studies. Br J Pain. 2017 Aug;11(3):119-133
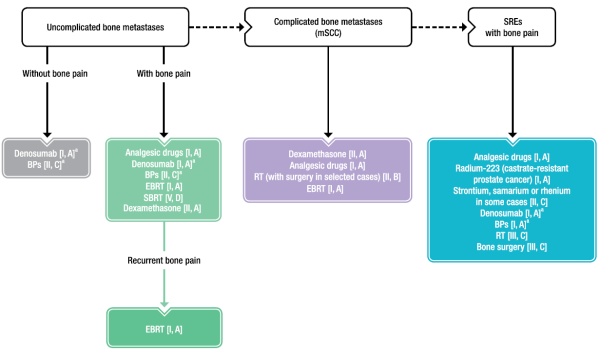
BONE PAIN & SPINAL CORD COMPRESSION /פרופסור פסח שוורצמן
- BTcP - breakthrough cancer pain;
- NSAIDs - nonsteroidal anti-inflammatory drugs
- BP - bisphosphonate;
- EBRT - external beam radiotherapy;
- HFRT - hypofractionated radiotherapy;
- mSCC - metastatic spinal cord compression;
- RT - radiotherapy;
- SBRT - stereotactic body radiotherapy;
- SRE - skeletal-related event
Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149–iv174.
a Do not switch between weak opioids
Remarks:
- NON-OPIOID ANALGESICS - See CHRONIC PAIN
- NSAIDS/COXIBs - See CHRONIC PAIN
- WEAK OPIOIDS - See CHRONIC PAIN
- STRONG OPIOIDS - See CHRONIC PAIN
- CANABIS - See CHRONIC PAIN
ALL OF THESE DRUGS ARE USED WHEN SKELETAL PAIN OR MSCC PAIN IS ACCOMPANIED BY AN ELEMENT OF NEUROPATHIC PAIN.
Comments:
- Most of the studies are Level 2 and not as cited in the ESMO paper
- The maximal dosage is the one that results in optimal pain relief with minimal adverse effects
- ביבליוגרפיה
- Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti Cl; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149-iv174.
- Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7:CD012592
- Schmidt-hansen M, Bromham N, Taubert M, Arnold S, Hilgart JS. Buprenorphine for treating cancer pain. Cochrane Database Syst Rev. 2015;(3]:CD009596
- Kane CM, Hoskin R Bennett Ml. Cancer induced bone pain. BMJ. 2015:350:11315־
- Von moos R, Body JJ, Egerdie B, et al. Pain and analgesic use associated with skeletal-related events in patients with advanced cancer and bone metastases. Support Care Cancer. 2016;24(3):1327-37.
- Tsuzuki S, Park SH, Eber MR, Peters CM, Shiozawa Y. Skeletal complications in cancer patients with bone metastases. Int J Urol. 2016;23(10):825-832
- De felice F, Piccioli A, Musio D, Tombolini V. The role of radiation therapy in bone metastases management. Oncotarget. 2017;8(15):25691-25699
- Ejima Y, Matsuo Y, Sasaki R. The current status and future of radiotherapy for spinal bone metastases. J Orthop Sci. 2015;20(4):585-92
- Israel JF, Parker G, Llack of benefit from paracetamol in palliative cancer patients reguiriing high doses of opioids: a randomised double blind placebo controlled trial, J Pain and Symptom Management, March 2010; 39(3]
- Gaertner JI, Stamer UM2, Remi C3, Voltz R4, Bausewein C3, Metamizole/dipyrone for the relief of cancer pain: A systematic review and evidence-based recommendations for clinical practice. Palliat Med. 2017 Jan; 31(1):26-34
- Levy M., Zylber-Katz E., Rosenkranz B., Clinical Pharmacokinetics of Dipyrone and its Metabolites, Clinical Pharmacokinetics. March 1995; 28(3):216-234
- Schmidt-Hansen M, Bennett Ml, Arnold S, Bromham N, Hilgart JS., Oxycodone for cancer-related pain. ,Cochrane Database of Systematic Reviews 2017, Issue 8
- Wiffen PJ, Wee B, Moore RA., Oral morphine for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 4
- M. Fa I Io n1, R. Giusti2, F. Aie 1113, P. H 0skin4, R. Rol ke 5, M. Sharma6 & C. I. Ripamo nti7, on behalf of the ESMO Guidelines Committee, Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Annals of Oncology 29 (Supplement 4): iv149-iv174,2018
- Straube C, Derry S, Jackson KG, Wiffen PJ, Bell RF, Strassels S, Straube S. Codeine, alone and with paracetamol (acetaminophen), for cancer pain.Cochrane Database of Systematic Reviews 2014, Issue 9
- Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT. Results of a Double- Blind, Randomized, Placebo-Controlled Study of Nabiximols Oromucosal Spray as an Adjunctive Therapy in Advanced Cancer Patients with Chronic Uncontrolled Pain, J Pain Symptom Manage. (Feb 2018): 55(2): 179-88
- Nicholson AB, Watson GR, Derry S, Wiffen PJ. Methadone for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 2
- Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain. Cochrane Database of Systematic Reviews 2013, Issue 10
- Corli 0, Floriani I, Roberto A, Montanari M, Galli F, Greco MT, Caraceni A, Kaasa S, Dragani TA, Azzarello G, Luzzani M, Cavanna L, Bandieri E, Gamucci T, Lipari G, Di Gregorio R, Valenti D, Reale C, Pavesi L, lorno V, Crispin0 C, Pacchioni M, ApoIone G; CERP STUDY OF PAIN GROUP: Are strong opioids equally effective and safe in the treatment of chronic cancer pain? A multicenter randomized phase IV 'real life' trial on the variability of response to opioids. Ann Oncol. (Jun 2016); 27(6): 1107-15
- Jandhyala R, Fullarton JR & Bennett ML Efficacy of Rapid-Onset Oral Fentanyl Formulations vs. Oral Morphine for Cancer- Related Breakthrough Pain: A Meta-Analysis of Comparative Trials. J Pain Symptom Management 2013 Oct; 46 (4): 573-80
- Mitchell A, McCrea R Inglis K, Porter G. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine (Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012 Nov; 19(12):3792-800
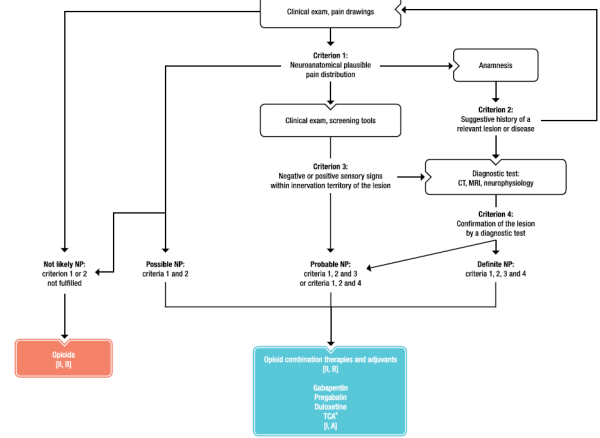
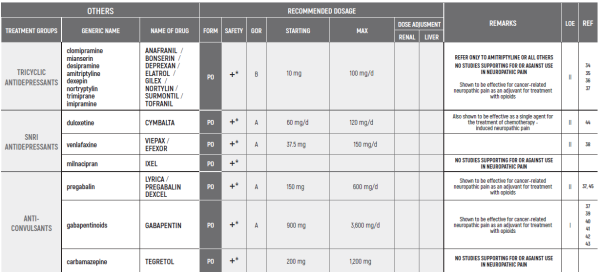
NEUROPATHIC PAIN/פרופסור עידו וולף
(*) TREATMENT OF ACUTE NEUROPATHIC PAIN
(direct nerve injury, e.g. celiac plexus involvement)
a Doses75 mg/day
- CT - computed tomography;
- MRI - magnetic resonance imaging;
- NP - neuropathic pain;
- TCA - tricyclic antidepressant
(*) Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149–iv174.
The section refers mostly to cancer-related neuropathic pain and not to chemotherapy induced neuropathic pain (CINP).
The only agent tested and found to be effective for chemotherapy induced neuropathic pain is duloxetine.
No intervention against non-painful chemotherapy induced neuropathy has been found to be effective.
- הערות
NON-OPIOID ANALGESICS - B,III
See CHRONIC PAIN
Dipyrone & paracetamol are often use for the treatment of neuropthic pain.
This is based on clinical experience and expert opinion.
NSAIDs/COXIBs - A,II
See CHRONIC PAIN
NSAIDs are often use for the treatment of neuropthic pain.
This is based on clinical experience and expert opinion.
WEAK OPIOIDS - A,II
See CHRONIC PAIN
Opioids are the mainstay of therapy for neuropathic pain. While this is based on older studies and lower level of evidence. This is based on vast clinical experience and expert guidelines as well as extrapolation from other pain syndromes.
STRONG OPIOIDS - A,II
See CHRONIC PAIN
Opioids are the mainstay of therapy for neuropathic pain. While this is based on older studies and lower level of evidence. This is based on vast clinical experience and expert guidelines as well as extrapolation from other pain syndromes.
CANABIS - C,V
See CHRONIC PAIN
While being used by many cancer patients, the efficacy of cannabis in the treatment of cancer-associated neuropathic pain has not been tested in clinical trials yet. Accumulating data suggest effect in non-cancer neuropathic pain.
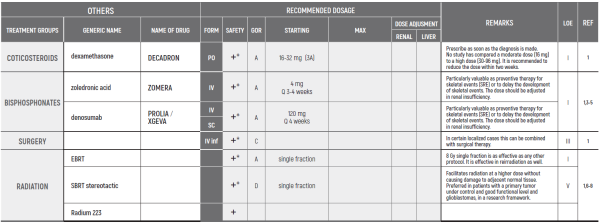
CORTICOSTEROIDS
Steroids are often use for acute severe neuropthic pain. This is based on clinical experience and expert opinion.
BENZODIAZEPINES - C,IV
Bezodiazepines have not been shown to be effective for cancer-associated neuropathic pain, although may be used to alleviate associated anxiety.
MEDICATIONS GIVEN AT SPECIALIZED CENTERS
Additional medications, mostly being used in specialized centers include ketamine, lidocaine...
LOCAL TREATMENTS
A wide array of local treatment modalities, conducted at specialized centers, should be considered. These include surgery, radiotherapy and nerve block.
- ביבליוגרפיה
- Leslie A. Shimp, Pharm.D., Safety Issues in the Pharmacologic Management of Chronic Pain in the Elderly. Pharmacotherapy 1998; 18(6): 1313-22
- https://www.drugs.com/dosage
- Cooper TE, Fisher E, Anderson B, Wilkinson NMR, Williams DG, Eccleston C, Paracetamol [acetaminophen) for chronic non-cancer pain in children and adolescents (Review), Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No.: CD012539
- Wiffen PJ, Derry S, Moore RA, McNicol ED, Bell RF, Carr DB, McIntyre M, Wee B. Oral paracetamol (acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No.: CD012637
- Israel JF, Parker G, Hack of benefit from paracetamol in palliative cancer patients reguiriing high doses of opioids: a randomised double blind placebo controlled trial, J Pain and Symptom Management, March 2010; 39(3)
- Gaertner )1, Stamer UM2, Remi 03, Voltz R4, Bausewein 03, Metamizole/dipyrone for the relief of cancer pain: A systematic review and evidence-based recommendations for clinical practice. Palliat Med. 2017 Jan; 31 (1): 26-34
- Levy M., Zylber-Katz E., Rosenkranz B., Clinical Pharmacokinetics of Dipyrone and its Metabolites, Clinical Pharmacokinetics. March 1995; 28(3): 216-234
- Mercandante S, Giarratano A.,: the long and winding road of non steroidal antinflammatory drugs and paracetamol in cancer pain management: A critical review Critical Reviews in On col ogy/H ematology, August 2013; 87(2): 140-5
- Derry S, Wiffen PJ, Moore RA, McNicol ED, Bell RF, Carr DB, McIntyre M, Wee B. Oral nonsteroidal anti-inflammatory drugs (NSAIDs) for cancer pain in adults. Cochrane Database of Systematic Reviews 2017, Issue 7.
- RA. Moore.,, aS. Derry,, PJ. Wiffen,, S. Straube,, DJ. Aldington, Overview review: Comparative efficacy of oral ibuprofen and paracetamol (acetaminophen) across acute and chronic pain conditions, Eur J Pain (2015); 19:1213-23
- Ventafridda V, De Conno F, Panerai AE, Maresca V, Monza GC, Ripamonti C. Non-steroidal anti-inflammatory drugs as the first step in cancer pain therapy: double-blind, within-patient study comparing nine drugs. JlntMed Res. (Jan-Feb 1990); 18(1): 21-9
- Ewan D McNicol Scott Strassel sLeonidas Goudas Joseph Lau Daniel B Carr: NSAIDS or paracetamol, alone or combined with opioids, for cancer pain, Cochrane Systematic Review: 20 April 2005
- Yalcin S, Altundag K, Asil M, Tekuseman G: Sublingual Piroxicam for cancer pain . Med Oncol (Jul 1998); 15(2): 137-9
- Bandieri E, Romero M, Ripamonti Cl, Artioli F, Sichetti D, Fanizza C, Santini D, Cavanna L, Melotti B, Conte PF, Roila F, Cascinu Bruera E, Tog non i G, Luppi M. Randomized Trial of Low-Dose Morphine Versus Weak Opioids in Moderate Cancer Pain. J Clin Oncol. (Feb 2016) 10; 34(5): 436-42
- Straube 0, Derry S, Jackson KO, Wiffen PJ, Bell RF, Strassels S, Straube S. Codeine, alone and with paracetamol (acetaminophen), for cancer pain.Cochrane Database of Systematic Reviews 2014, Issue 9
- Eisenberg E1, Berkey CS, Carr DB, Mosteller F, Chalmers TC., Efficacy and safety of nonsteroidal antiinflammatory drugs for cancer pain: a meta-analysis. J Clin Oncol. (Dec 1994); 12(12): 2756-65
- Wiffen PJ, Derry S, Moore RA. ramadol with or without paracetamol (acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 5
- Schmidt-Hansen M, Bromham N, Taubert M, Arnold S, Hilgart JSSchmidt-Hansen M, Bromham N, Taubert M, Arnold S, Hilgart JS. Buprenorphine for treating cancer pain .Cochrane Database of Systematic Reviews 2015, Issue 3.
- Schmidt-Hansen M, Bennett Ml, Arnold S, Bromham N, Hilgart JS., Oxycodone for cancer-related pain. ,Cochrane Database of Systematic Reviews 2017, Issue 8.
- Wiffen PJ, Wee B, Moore RA., Oral morphine for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 4.
- Nicholson AB, Watson GR, Derry S, Wiffen PJ. Methadone for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 2
- Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain. Cochrane Database of Systematic Reviews 2013, Issue 10
- Corli 0, Floriani I, Roberto A, Montanari M, Galli F, Greco MT, Caraceni A, Kaasa S, Dragani TA, Azzarello G, Luzzani M, Cavanna L, Bandieri E, Gamucci T, Lipari G, Di Gregorio R, Valenti D, Reale C, Pavesi L, lorno V Crispino C, Pacchioni M, ApoIone G; CERP STUDY OF PAIN GROUP: Are strong opioids egually effective and safe in the treatment of chronic cancer pain? A multicenter randomized phase IV 'real life' trial on the variability of response to opioids. Ann Oncol. (Jun 2016); 27(6): 1107-15
- Sande TA, Laird BJ, Fallon MT, The use of opioids in cancer patients with renal impairment-a systematic review, Support Care Cancer. (Feb 2017); 25(2): 661-75
- King S, Forbes K, Flanks GW, Ferro CJ, Chambers EJ., A systematic review of the use of opioid medication for those with moderate to severe cancer pain and renal impairment: a European Palliative Care Research Collaborative opioid guidelines project. Palliat Med.(Jul 2011); 25(5): 525-52
- Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti Cl; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149-iv174.
- Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT. Results of a Double- Blind, Randomized, Placebo-Controlled Study of Nabiximols Oromucosal Spray as an Adjunctive Therapy in Advanced Cancer Patients with Chronic Uncontrolled Pain, J Pain Symptom Manage. (Feb 2018): 55(2): 179-88
- Jandhyala R, Fullarton JR & Bennett Ml. Efficacy of Rapid-Onset Oral Fentanyl Formulations vs. Oral Morphine for Cancer- Related Breakthrough Pain: A Meta-Analysis of Comparative Trials. J Pain Symptom Management 2013 Oct; 46 (4): 573-80
- Arbaiza D1, Vidal 0. Tramadol in the treatment of neuropathic cancer pain: a double-blind, placebo-controlled study. Clin Drug Investig. 2007; 27(1):75-83
- Dellemijn PL et al. Medical therapy of malignant nerve pain. A randomised double-blind explanatory trial with naproxen versus slow-release morphine. Eur J Cancer, 30A (1994); V 30, Issue 9:1244-1250
- Jongen JL et al. The evidence for pharmacologic treatment of neuropathic cancer pain: beneficial and adverse effects. J Pain Symptom Manage. 2013 Oct; 46(4):581-590
- Mishra S, Bhatnagar S et al. Management of neuropathic cancer pain following WHO analgesic ladder: a prospective study. Am J Hosp Palliat Care. 2008 Dec-2009 Jan;25(6):447-51
- Ong E.C. Controlled-Release Oxycodone in the Treatment of Neuropathic Pain of Nonmalignant and Malignant Causes. Oncology 2008;74:72-75
- Kalso E et al. Amitriptyline effectively relieves neuropathic pain following treatment of breast cancer. Pain. 1996 Feb; 64(2):293-302
- Mercadante S et al. Amitriptyline in Neuropathic Cancer Pain in Patients on Morphine Therapy: A Randomized Placebo- controlled, Double-blind Crossover Study. Tumori May 2002; 88(3):239-42
- Kautio AL et al. Amitriptyline in the treatment of chemotherapy-induced neuropathic symptoms. J Pain Symptom Manage. 2008 Jan; 35(1):31-9
- Mishra S et al. A comparative efficacy of amitriptyline, gabapentin, and pregabalin in neuropathic cancer pain: a prospective randomized double-blind placebo-controlled study. Am J Hosp Palliat Care. 2012 May; 29(3):177-82
- Tasmuth T et al. Venlafaxine in neuropathic pain following treatment of breast cancer. Eur J Pain. 2002; 6(1):17-24
- A. Caraceni et al. Gabapentin for neuropathic cancer pain: a randomized controlled trial from the Gabapentin Cancer Pain Study Group. J Clin Oncol. 2004 Jul 15; 22(14):2909-17
- Rao RD et al. Efficacy of gabapentin in the management of chemotherapy-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled, crossover trial (N00C3). Cancer. 2007 Nov 1; 110(9):2110-8
- Keskinbora K et al. Gabapentin and an opioid combination versus opioid alone for the management of neuropathic cancer pain: a randomized open trial. J Pain Symptom Manage. 2007 Aug; 34(2):183-9
- Tsavaris N et al. Gabapentin monotherapy for the treatment of chemotherapy-induced neuropathic pain: a pilot study. Pain Med. 2008 Nov; 9(8):1209-16
- Ross JR et al. Gabapentin is effective in the treatment of cancer-related neuropathic pain: a prospective, open-label study. J Palliat Med. 2005 Dec;8(6):1118-26
- Smith EM, Pang H et al. Effect of duloxetine on pain, function, and guality of life among patients with chemotherapy- induced painful peripheral neuropathy: a randomized clinical trial. JAMA. 2013 Apr 3;309(13):1359-67
- Jiang J, Li Y et al. Effect of Pregabalin on Radiotherapy-Related Neuropathic Pain in Patients With Head and Neck Cancer: A Randomized Controlled Trial. J Clin Oncol. 2018 Nov 20JCO1800896.
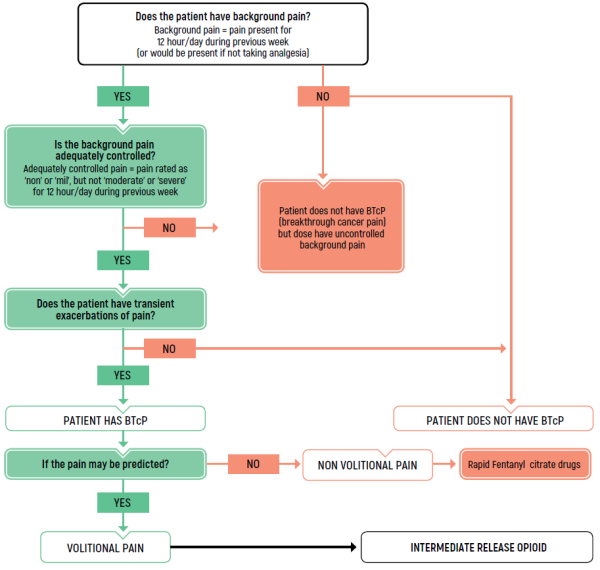
BREAKTHROUGH PAIN/ד"ר דניאלה זלמן
TREATMENT OF BREAKTHROUGH PAIN
Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149-iv174.
BTcP - breakthrough cancer pain
LIMITED USE FOR SHORT PERIODS ONLY RESPONDING PATIENTS: RE EVALUATE FOR LONG TERM USE RISK FACTORS
CANABIS:
SATIVEX is indicated as adjunctive treatment for the symptomatic relief of neuropathic pain in multiple sclerosis in adults.
SATIVEX may be useful as adjunctive analgesic treatment in adult patients with advanced cancer who experience moderate to severe pain during the highest tolerated dose of strong opioid therapy for persistent background pain.
The indications in the Ministry of Health’s “Procedure 106” are:
2.3.0.0. For patients during treatment with chemotherapy and up to six months after its completion to relieve nausea, vomiting, or pain related to treatment (even without exhaustion of conventional treatments for relief of nausea, etc.). In cases where the attending physician believes cannabis treatment should be continued after half a year- he will specify the reasons for the continuation of the treatment and for what period he believes the treatment should be continued
2.3.0.3. To relieve pain from a cancerous source at the metastatic stage and after exhausting conventional treatment options
- ביבליוגרפיה
- Gelot S, Nakhla E. Opioid dosing in renal and hepatic failure. US Pharmacist 2014;39(8):34-38.
- Daeninck P Gagnon B, Gallagher R, Henderson JD, Shir Y, Zimmermann C, Lapointe B. Canadian recommendations for the management of breakthrough cancer pain. Curr Oncol, 2016 Apr;23(2):96-108.
- Davies AN, Dickman A, Reid C, Stevens AM, Zeppetella G on behalf of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain 2009;13:331-8.
- Fallon M, Giusti R, Aielli F, Hoskin P Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv166-iv191.
- Wiffen PI, Wee B, Derry S et al. Opiod for cancer pain - an overview of the Cochrane review. Cochrane Database Syst Rev 2017: 7; CD012592.
- Lobre ET, Klepstad P Bennet MI et al. From “breakthrough” to “episodic” cancer pain? A European association for palliative care research network expert Delphi survey common a terminology and classification of transient of cancer pain exacerbation. J Pain Symp Manag, 2016, 51: 1013-1019.
- www.drugs.com - Micromedex (A to Z) Professional.
- Fallon M, Giusti R, Aielli F, Hoskin P Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149-iv174.
- Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT Results of a Double-Blind, Randomized, Placebo-Controlled Study of Nabiximols Oromucosal Spray as an Adjunctive Therapy in Advanced Cancer Patients with Chronic Uncontrolled Pain, J Pain Symptom Manage. (Feb 2018): 55(2): 179-88
- Fallon MT, Albert Lux E, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Lichtman AH & Kornyeyeva E. Sativex oromucosal spray as adjunctive therapy in advanced cancer patients with chronic pain unalleviated by optimized opioid therapy: two double-blind, randomized, placebo-controlled phase 3 studies. Br J Pain. 2017 Aug;11(3):119-133
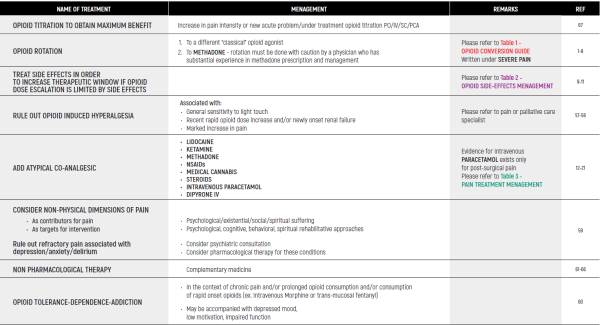
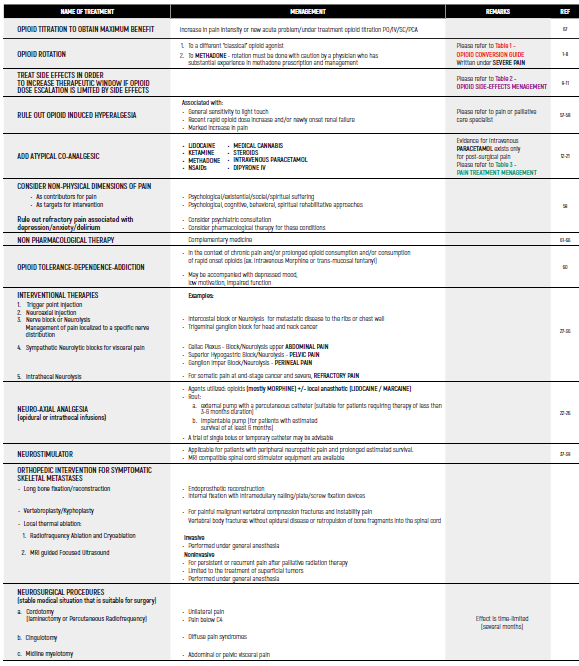
OPIOID - REFRACTORY & RESISTANT PAIN/ד"ר איריס גלוק, ד"ר אופיר מורג, ד"ר יקיר רוטנברג
APPROACH TO THE TREATMENT OF REFRACTORY & RESISTANT PAIN
(Not adequately alleviated by a strong opioid agonists, despite appropriate dose titration, at a tolerable, safe dose)
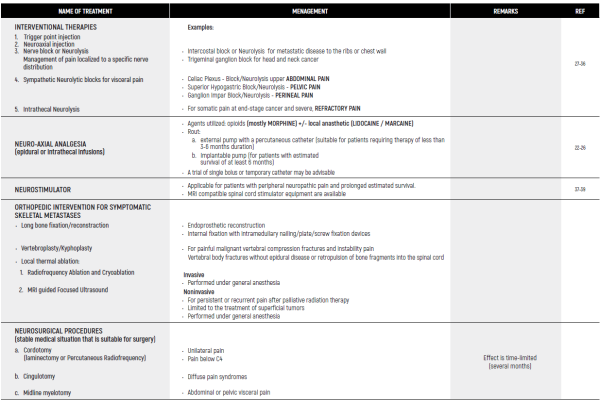
APPROACH TO THE TREATMENT OF REFRACTORY & RESISTANT PAIN - INTERVENTIONAL THERAPIES
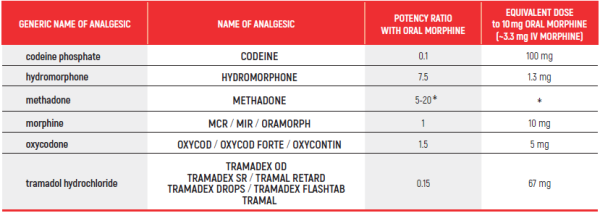
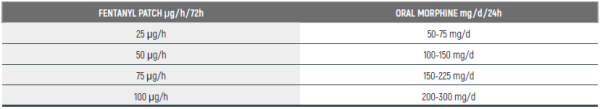
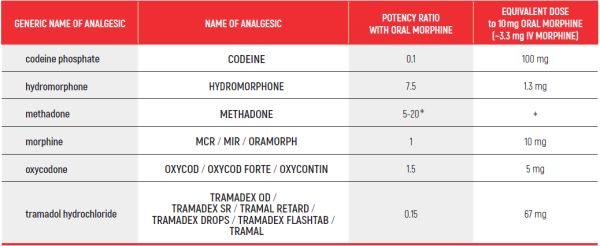
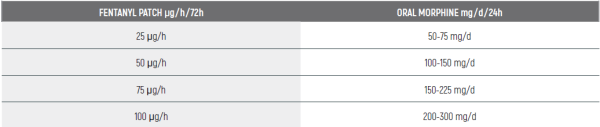
OPIOID CONVERSION GUIDE - Table 1
Opioid Conversion Guide:
The relative potency of methadone depends on the starting dose and the duration of administration. Conversions to and from methadone should always be undertaken with specialist advice
Fentanyl to Morphine Conversion Guide:
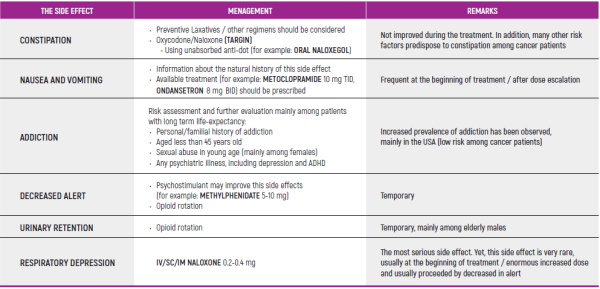
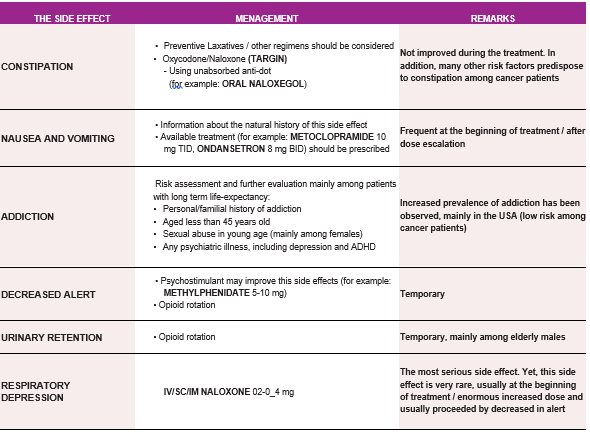
OPIOID SIDE EFFECTS MENAGEMENT - Table 2
(*) Patients should be informed, empowered and encouraged to communicate with the medical staff about side effects. Most of opioid’s side effects are improved within a few days, except for constipation. In case of resistance side effects, option of decreasing dose and/or opioids rotation should be considered.
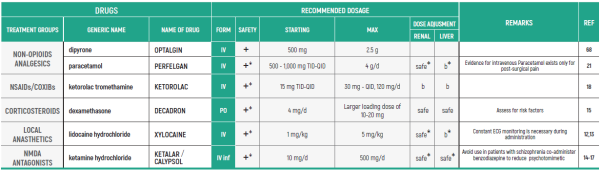
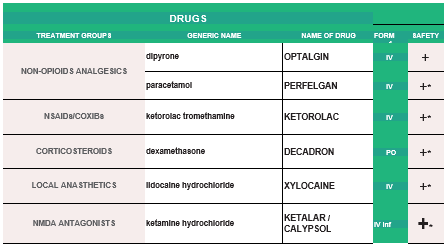
PAIN TREATMENT MENAGEMENT - Table 3
Remarks:
PARACETAMOL
- Avoid long-term administration of more than 4 g/d.
LIDOCAINE
- Constant ECG (Electrocardiography) monitoring is necessary during IV administration
- Use is contraindicated in patients with Wolff-Parkinson-White syndrome and severe degrees of SA, AV, or intraventricular heart block (except in patients with a functioning artificial pacemaker)
- Correct hypokalemia or hypomagnesemia, prior to using
- Reduce dose in hepatic dysfunction and CHF (Chronic Heart Failure)
KETAMINE
- Use with caution in patients with coronary artery disease, hypertension and tachycardia
Ketamine increases blood pressure, heart rate and cardiac output thereby increasing myocardial oxygen demand
- Cerebrospinal fluid (CSF) pressure elevation/brain metastasis
- Avoided in patients 65 years and older due to an increased risk of GI bleeding, peptic ulcer disease, and acute kidney injury. May decline kidney function
- Contraindicated in patients with advanced renal impairment and in patients at risk for renal failure due to volume depletion
- Avoid use in patients with active GI bleeding. Use caution with a history of GI ulcers, inflammatory bowel disease, concurrent therapy known to increase the risk of GI bleeding
- Dosage adjustment is required in patients with moderate elevation in serum creatinine
Assess for risk factors for complications — preexisting conditions should be assessed:
- Diabetes mellitus
- Poorly controlled hypertension
- Heart failure and peripheral edema
- Glaucoma
- Peptic ulcer disease. Patients who also require concomitant treatment with nonsteroidal antiinflammatory drugs (NSAIDs) or anticoagulants may require prophylaxis to prevent gastroduodenal toxicity
- ביבליוגרפיה
- Indelicato RA, Portenoy RK. Opioid rotation in the management of refractory cancer pain. J Clin Oncol 2002; 20:348.
- Fine PG, Portenoy RK, Ad Hoc Expert Panel on Evidence Review and Guidelines for Opioid Rotation. Establishing "best practices' for opioid rotation: conclusions of an expert panel. J Pain Symptom Manage 2009; 38:418.
- Chatham MS, Dodds Ashley ES, Svengsouk JS, Juba KM. Dose ratios between high dose oral morphine or eguivalents and oral methadone. J Palliat Med 2013; 16:947.
- Mercadante S, Casuccio A, Fulfaro F, et al. Switching from morphine to methadone to improve analgesia and tolerability in cancer patients: a prospective study. J Clin Oncol 2001; 19:2898.
- Mercadante S CasuccioA Calderone L.Rapid switching from morphine to methadone in cancer patients with poor response to morphine J Clin Oncol 1999:3307 3312
- Parsons HA, de la Cruz M, El Osta B, et al. Methadone initiation and rotation in the outpatient setting for patients with cancer pain. Cancer 2010:116:520.
- McLean S, Twomey F. Methods of Rotation From Another Strong Opioid to Methadone for the Management of Cancer Pain: A Systematic Review of the Available Evidence. J Pain Symptom Manage 2015; 50:248.
- Mercadante s, BrueraE.Opioid switching in cancer pain: from the beginning to nowadays. Crit Rev Oncol Hematol2016; 99:241-24
- Cherny N, Ripamonti C Strategies to manage the adverse effects of oral morphine: an evidence-based report.Expert Working Group of the European Association of Palliative Care Network.] Clin Oncol. 2001 May 1;19[9):2542-54. Review
- Benyamin R,Trescot AM DattaS et al. Opioid complicationsand side effects Pain Physician 2008:11(2 Suppl): S105-S12
- StoneR MintonO.European Palliative Care Research collaborative pain guidelines. Central side-effects management: what is the evidence to support best practice in the management of sedation, cognitive impairment and myoclonus? Palliat Med2011; 25: 431-441
- Challapalli V, Tremont-Lukats IW, McNicol ED, et al. Systemic administration of local anesthetic agents to relieve neuropathic pain. Cochrane Database Syst Rev 2005; :CD003345.
- Buchanan DD, J Maclvor F. A role for intravenous lidocaine in severe cancer-related neuropathic pain at the end-of-life. Support Care Cancer 2010:18:899.
- Bell RF, Eccleston C, Kalso EA. Ketamine as an adjuvant to opioids for cancer pain. Cochrane Database Syst Rev 2017; 6: CD003351
- Ben-Ari A, Lewis MC, Davidson E. Chronic administration of ketamine for analgesia. J Pain Palliat Care Pharmacother 2 007; 21:7.
- Jackson K, Ashby M, Howell D, et al. The effectiveness and adverse effects profile of "burst‘ ketamine in refractory cancer pain: The VCOG PM 1-00 study. J Palliat Care 2010; 26:176.
- Prommer EE. Ketamine for pain: an update of uses in palliative care. J Palliat Med 2012; 15:474.
- DerryS, Wiffen PJ, MooreRet al. Oral nonsteroidal anti-inflammatory drugs [NSAIDs] for cancer pain in adults. Cochrane Database Syst Rev2017; 12: CD012638
- JohnsonJR, Burnell-Nugen et al. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC: cBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manage 2010; 39; :167-179
- Vu Bach T et al .Use of Methadone as an Adjuvant Medication to Low-Dose Opioids for Neuropathic Pain in the Frail Elderly: A Case Series. J Palliat Med. 2016 Dec;19(12):1351-1355. Epub 2016 Oct 11.
- Jibril F, Sharaby S, Mohamed A, Wilby KJ. Intravenous versus Oral Acetaminophen for Pain: Systematic Review of Current Evidence to Support Clinical Decision-Making. Can J Hosp Pharm. 2015;68[3):238-47.
- VainioA, Tigerstedtl. Opioid treatment for radiating cancer pain: oral administration vs. epidural technigues. Acta Anaesthesiol Scand1988; 32:179-185
- Deer TR, Prager J, Levy R, et al. Polyanalgesic Consensus Conference 2012: recommendations for the management of pain by intrathecal (intraspinal) drug delivery: report of an interdisciplinary expert panel. Neuromodulation 2012; 15:436.
- Birthi P, Sloan P. Interventional treatment of refractory cancer pain. Cancer J 2013; 19:390.
- Mercadante S, Intravaia G, Villari P, et al. Intrathecal treatment in cancer patients unresponsive to multiple trials of systemic opioids. Clin J Pain 2 007; 23:793.
- The effectiveness of subcutaneously implanted epidural ports for relief of severe pain in patients with advanced-stage gynecological cancer: a prospective study.Ertag IE et al. Agri. [2014]
- Chambers WA. Nerve blocks in palliative care. Br J Anaesth 2008; 101:95.
- Burton, AW, Phan, et al. Treatment of cancer pain: Role of neural blockade and neuromodulation. In: Cousins and Bridenbaugh's Neural Blockade in Clinical Anesthesia and Pain Medicine, 4th, Lippincott, Williams & Wilkins, 2009. p.1122.
- Lerna, MJ. Invasive procedures for cancer pain. Pain: Clinical Updates; 6:1. International Association for the Study of Pain [ IASP) available online at http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=Home&TEMPLATE=/CM/ContentDisplay. cfm&CONTENTID=7603 [Accessed on August 30,2010).
- Arcidiacono PG, Calori G, Carrara S, et al. Celiac plexus block for pancreatic cancer pain in adults. Cochrane Database Syst Rev 2011; :CD 007519.
- Amr YM, Makharita MY. Neurolytic sympathectomy in the management of cancer pain-time effect: a prospective, randomized multicenter study. J Pain Symptom Manage 2014; 48:944.
- Plancarte R, de Leon-Casasola GA, El-Helaly M, et al. Neurolytic superior hypogastric plexus block for chronic pelvic pain associated with cancer. Reg Anesth 1997; 22:562.
- de Leon-Casasola GA, Kent E, Lerna MJ. Neurolytic superior hypogastric plexus block for chronic pelvic pain associated with cancer. Pain 1993; 54:145.
- Interventional Treatments of Cancer Pain.Sindt JE et al. Anesthesiol Clin. [2016]
- Intercostal Nerve Block and Neurolysis for Intractable Cancer Pain.Matchett G et al. J Pain Palliat Care Pharmacother. [2016]
- The Effectiveness of Alcohol Versus Phenol Based Splanchnic Nerve Neurolysis for the Treatment of Intra-Abdominal Cancer Pain.Koyyalagunta D etal. Pain Physician. [2016]
- National Institute for Health and Care Excellence [NICE] Spinal Cord Stimulation for Chronic Pain of Neuropathic or Ischaemic Origin. NICE Technology Appraisal Guidance TA 159, Published 22nd October 2008. www.nice.org.uk/guidance/ta159 [11 April 2018, date last accessed).172
- PengL, MinS, ZejunZet al. Spinal cord stimulation for cancer-related pain in adult. Cochrane Database Syst Rev2015;CD009389
- 173British Thoracic Society Standards of Care CommitteeBTS statement on malignant mesothelioma in the UK, 2 007. Thorax2007; 62[Suppl 2):ii1-ii19
- Percutaneous cervical cordotomy in cancer pain.Bellini M, Barbieri M.Anaesthesiol Intensive Ther. 2016;48[3):197-200. doi: 10.5603/ AIT.a2014.0070. Epub 2014 Dec 19. Review.
- Palliative CT-Guided Cordotomy for Medically Intractable Pain in Patients with Cancer.Shepherd TM, Hoch MJ, Cohen BA, Bruno MT, Fieremans E, Rosen G, Pacione D, Mogilner AY.AJNR Am J Neuroradiol. 2017 Feb;38[2):387-390
- DREZotomy in the treatment of cancer pain: a review.Gadgil N, Viswanathan AStereotact Fund Neurosurg. 2012;90[6):356-60. doi: 10.1159/000341072. Epub 2012 Aug 23. Review.
- Double Anterior Stereotactic Cingulotomy for Intractable Oncological Pain.Strauss I, Berger A, Ben Moshe S, Arad M, Hochberg U, Gonen T,Tellem R.Stereotad Fund Neurosurg. 2017;95[6):400-408
- Cingulotomy for medically refractory cancer pain.Viswanathan A, Harsh V, Pereira EA, Aziz TZNeurosurg Focus. 2013 Sep;35(3]:E1
- Health Quality Ontario. Vertebral Augmentation Involving Vertebroplasty or Kyphoplasty for Cancer-Related Vertebral Compression Fractures: A Systematic Review. Ont Health Technol Assess Ser 2016; 16:1.
- Lutz S, Balboni T, Jones J, et al. Palliative radiation therapy for bone metastases: Update of an ASTRO Evidence-Based Guideline. Prad Radiat Oncol 2017; 7:4.
- Solberg J, Copenhaver D, Fishman SM. Medial branch nerve block and ablation as a novel approach to pain related to vertebral compression fracture. Curr Opin Anaesthesiol 2016; 29:596.
- Hong D, Andren-Sandberg A. Punctate midline myelotomy: a minimally invasive procedure for the treatment of pain in inextirpable abdominal and pelvic cancer. J Pain Symptom Manage 20 07; 33:99.
- Ferrante FM. Neuraxial infusion in the management of cancer pain. Oncology [Williston Park) 1999; 13:30.
- Smith TJ, Staats PS, Deer T, et al. Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol 2002; 20:4040.
- Peng L, Min S, Zejun Z, et al. Spinal cord stimulation for cancer-related pain in adults. Cochrane Database Syst Rev 2015; CD009389.
- Brogan S, Junkins S. Interventional therapies for the management of cancer pain. J Support Oncol 2010; 8:52.
- Alireza Feizerfan, JHL Antrobus; Role of percutaneous cervical cordotomy in cancer pain management, Continuing Education in Anaesthesia Critical Care & Pain, Volume 14, Issue 1,1 February 2014, Pages 23-26, https://doi.org/10.1093/bjaceaccp/mkt033
- Wood TJ, Racano A, Yeung H, et al. Surgical management of bone metastases: guality of evidence and systematic review. Ann Surg Oncol 2014; 21:4081
- Dababou S, Marrocchio 0, Scipione R, Erasmus HP, Ghanouni R Anzidei M, Catalano C, Napoli A. High-Intensity Focused Ultrasound for Pain Management in Patients with Cancer. Radiographics. 2018 Mar-Apr;38[2):603-623. doi: 10.1148/rg.2018170129. Epub 2018 Jan 30.,
- Harding D et al Evaluation of Quality of Life Outcomes Following Palliative Treatment of Bone Metastaseswith Magnetic Resonance-guided High Intensity Focused Ultrasound: An International Multicentre Study. Clin Oncol [R Coll Radiol). 2018 Apr;30(4):233-242. doi: 10.1016/j.clon.2017.12.023. Epub 2018 Jan 6.
- Is opioid-induced hyperalgesia a genuine issue for palliative care patients and clinician's ?Peter Eastman, Brian H. Le, Ian Grant, and Sue Berry Journal of Clinical Oncology 2014 32:31_suppi, 197-197
- L. A. Colvin, M. T. Fallon; Opioid-induced hyperalgesia: a clinical challenge, BJA: British Journal of Anaesthesia, Volume 104, Issue 2,1 February 2010, Pages 125-127
- Breitbart, W. [1989], Psychiatric management of cancer pain. Cancer, 63:2336-2342.
- Responsible, Safe, and Effective Prescription of Opioids for Chronic Non-Cancer Pain: American Society of Interventional Pain Physicians (ASIPP) GuidelinesLaxmaiah Manchikanti, Adam Marc Kaye, J A Hirsch Pain physician 2017
- Paley CA, Johnson MIJashani 0A, Bagnall AM. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev 2015;CD007753.
- The Institute for Alternative and Complementary Medicine http://shrp.umdnj.edu/programs/ICAM/ [Accessed on February 21, 2012).
- Bardia A, Barton DL, Prokop LJ, et al. Efficacy of complementary and alternative medicine therapies in relieving cancer pain: a systematic review. J Clin Oncol 2006; 24:5457
- Boyd 0, Crawford C, Paat CF, et al. The impact of massage on function in pain population - a systematic review and meta-analysis of randomized controlled trials: part II, Cancer pain populations. Pain Med 2016; 17[8):1553-1568.
- Lee SH, Kim JY, Yeo S et al. Meta-analysis of massage therapy on cancer pain. Integr Cancer Ther 2015; 14[4):297-304
- Strouse TB, Bursch B. Psychological treatment. Hematol Oncol Clin North Am. 2018; 32[3):483-491
- Mercadante S. Opioid titration in cancer pain: a critical review. Eur J Pain. 2007 Nov;11[8):823-30
- Gaertner J, Stamer UM et al. Metamizole/dipyrone for the relief of cancer pain: A systematic review and evidence-based recommendations for clinical practice. Palliat Med. 2017 Jan;31[1):26-34.
PHARMACOLOGICAL PAIN TREATMENT IN ADULTS ONCOLOGY
(*) NSAIDs: LIMITED USE FOR SHORT PERIODS ONLY RESPONDING PATIENTS: RE EVALUATE FOR LONG TERM USE RISK FACTORS
- הערות
(*) ALL PRODUCT USE ARE BY SmPC
NON-OPIOID ANALGESICS - B,III
1. PARACETAMOL: Avoid long-term administration of more than 4 g/d. Avoid when patient is ingesting limited food or consumes long-term ethanol
2. DIPYRONE/MITAMIZOLE: Agranulocytosis has been described with varying relative risks in different populations. Patients should be advised to seek for medical care if signs of infection
NSAIDs
3. Prolonged use not advised due to concern of side effects such as hypertension, edema, CVD, GI bleeding, renal toxicity and bleeding diathesis weak opioids
WEAK OPIOIDS
4. Ceiling effect may reduce efficacy and induce side effects
6. Use with caution with other paracetamol containing products
STRONG OPIOIDS:
8. Beware in elderly - may develop confusion
9. Discontinuation should be gradual to avoid withdrawal symptoms
10. METHADONE is equivalent to morphine in terms of efficacy but needs careful titration. Half-life may differ between people - careful titration needed. Advised to be used by experts only
OTHERS:
CANABIS:
- While being used by many cancer patients, the efficacy of cannabis in the treatment of cancer-associated neuropathic pain has not been tested in clinical trials yet. Accumulating data suggest effect in non-cancer neuropathic pain.
CORTICOSTEROIDS
- Steroids are often use for acute severe neuropthic pain. This is based on clinical experience and expert opinion.
BENZODIAZEPINES
- Bezodiazepines have not been shown to be effective for cancer-associated neuropathic pain, although may be used to alleviate associated anxiety.
MEDICATIONS GIVEN AT SPECIALIZED CENTERS
- Additional medications, mostly being used in specialized centers include ketamine, lidocaine.
LOCAL TREATMENTS
- A wide array of local treatment modalities, conducted at specialized centers, should be considered. These include surgery, radiotherapy and nerve block
PHARMACOLOGICAL PAIN TREATMENT IN ADULTS ONCOLOGY/ OPIOID - Refractory & Resistant Pain
APPROACH TO THE TREATMENT OF REFRACTORY PAIN (Not adequately alleviated by a strong opioid agonists, despite appropriate dose titration, at a tolerable, safe dose)
Dr Gluck I., Dr Morag O.
OPIOID CONVERSION GUIDE - Table 1 - Dr Rottenberg Y.
Opioid Conversion Guide:
The relative potency of methadone depends on the starting dose and the duration of administration. Conversions to and from methadone should always be undertaken with specialist advice
Fentanyl to Morphine Conversion Guide:
OPIOID SIDE EFFECTS MENAGEMENT - Table 2 - Dr Rottenberg Y.
Patients should be informed, empowered and encouraged to communicate with the medical staff about side effects. Most of opiod’s side effects are improved within a few days, except for constipation. In case of resistance side effects, option of decreasing dose and/or opioids rotation should be considered
PAIN TREATMENT MENAGEMENT - Table 3 - Dr Gluck I., Dr Morag O.
- הערות
PARACETAMOL
- Avoid long-term administration of more than 4 g/d.
LIDOCAINE
- Constant ECG monitoring is necessary during IV administration
- Use is contraindicated in patients with Wolff-Parkinson-White syndrome and severe degrees of SA, AV, or intraventricular heart block (except in patients with a functioning artificial pacemaker)
- Correct hypokalemia or hypomagnesemia, prior to using
- Reduce dose in hepatic dysfunction and CHF.
KETAMINE
- Use with caution in patients with coronary artery disease, hypertension and tachycardia. Ketamine increases blood pressure, heart rate and cardiac output thereby increasing myocardial oxygen demand
- Cerebrospinal fluid (CSF) pressure elevation/brain metastasis.
KETOROLAC
- Avoided in patients 65 years and older due to an increased risk of GI bleeding, peptic ulcer disease, and acute kidney injury. May decline kidney function
- Contraindicated in patients with advanced renal impairment and in patients at risk for renal failure due to volume depletion
- Avoid use in patients with active GI bleeding. Use caution with a history of GI ulcers, inflammatory bowel disease, concurrent therapy known to increase the risk of GI bleeding
- Dosage adjustment is required in patients with moderate elevation in serum creatinine.
DEXAMETHASONE
Assess for risk factors for complications — preexisting conditions should be assessed:
- Diabetes mellitus
- Poorly controlled hypertension
- Heart failure and peripheral edema
- Glaucoma
- Peptic ulcer disease.Patients who also require concomitant treatment with nonsteroidal antiinflammatory drugs (NSAIDs) or anticoagulants may require prophylaxis to prevent gastroduodenal toxicity
- ALL PRODUCT USE ARE BY SmPC
איגודים משתתפים
- אגודה ישראלית לכאב
- האיגוד הישראלי לאונקולוגיה קלינית ורדיותרפיה
- האיגוד הישראלי להמטולוגיה ואונקולוגיה ילדים
- האיגוד לרפואה פליאטיבית בישראל
- האיגוד הישראלי לרפואה פנימית
- החוג לטיפול בכאב של איגוד רופאי המשפחה
- איגוד הכירורגים בישראל
- האיגוד הישראלי לאורתופדיה
- האיגוד הישראלי לפרמקולוגיה קלינית - רפואה, ייעוץ ומחקר בתרופות
העורכים
- פרופסור אליעד דוידסון - יו"ר האגודה הישראלית לכאב, מנהל היחידה לשיכוך כאב, המרכז הרפואי הדסה עין-כרם
- ד"ר וילמוש מרמרשטיין - יו"ר האיגוד הישראלי לאונקולוגיה קלינית ורדיותרפיה
- ד"ר יקיר רוטנברג - יו"ר האיגוד הפליאטיבי באיגוד הישראלי לאונקולוגיה קלינית ורדיותרפיה, מח׳ אונקולוגית, המרכז הרפואי הדסה עין-כרם
- פרופסור פסח שוורצמן - יו"ר האיגוד הישראלי לרפואה פליאטיבית, מנהל יחידה פליאטיבית, המרכז הרפואי האוניברסיטאי סורוקה
- פרופסור עידו וולף - מנהל המערך האונקולוגי, המרכז הרפואי ת"א
- ד"ר אורה רוזנגרטן - מנהלת היח׳ לאונקולוגיה גניקולוגית, המרכז הרפואי שערי צדק
- ד"ר דניאלה זלמן - רופאה בכירה, אחראית מחלקת אשפוז רדיותרפיה, המערך האונקולוגי, המרכז הרפואי רמב"ם
- ד"ר איריס גלוק - מנהלת המערך לטיפול תומך, מומחית באונקולוגיה ובטיפול תומך, המרכז הרפואי ע"ש חיים שיבא, תה"ש
- ד"ר אופיר מורג - מנהלת מרפאת כאב אונקולוגי, מומחית ברפואת שיכוך כאב ואונקולוגיה רפואית, המרכז הרפואי ע"ש חיים שיבא, תה"ש
- ד"ר סילביו בריל - מנהל המכון לשיכוך כאב, המרכז הרפואי ת"א
- ד"ר איתי גור-אריה - מנהל המכון לשיכוך כאב, המרכז הרפואי ע"ש חיים שיבא, תה"ש
- פרופסור אילון איזנברג - מנהל היחידה לחקר הכאב, המרכז הרפואי רמב"ם
- פרופסור משה סלעי - מנהל החטיבה האורתופדית, המרכז הרפואי ת"א
- פרופסור אבישי אליס - יו"ר האיגוד הישראלי לרפואה פנימית, מנהל מח׳ פנימית ג', המרכז הרפואי רבין, ביה"ח בילינסון
- פרופסור גיל בר-סלע - מנהל המרכז למחלות סרטן, מרכז רפואי העמק
- ד"ר מיכל שני - יו"ר האיגוד הישראלי לרפואת משפחה
- ד"ר ורד סימוביץ - יו"ר החוג לטיפול בכאב, איגוד רופאי המשפחה בישראל, מומחית ברפואת משפחה, מנהלת רפואית של חטיבת התפעול, מכבי שירותי בריאות


 כניסה
כניסה  עקבו אחרינו בפייסבוק
עקבו אחרינו בפייסבוק