הבדלים בין גרסאות בדף "אמנות הטיפול התרופתי בכאב בחולה האונקולוגי המבוגר - נייר עמדה - Pharmacological pain treatment in adults oncology"
| שורה 225: | שורה 225: | ||
;ביבליוגרפיה: | ;ביבליוגרפיה: | ||
| + | <div style="text-align: left; direction: ltr"> | ||
| + | |||
#Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti Cl; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol [2018);29 [Suppl 4): iv149-iv174. | #Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti Cl; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol [2018);29 [Suppl 4): iv149-iv174. | ||
#Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7:CD012592 | #Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7:CD012592 | ||
| שורה 237: | שורה 239: | ||
#Levy M., Zylber-Katz E., Rosenkranz B., Clinical Pharmacokinetics of Dipyrone and its Metabolites, Clinical Pharmacokinetics. March 1995; 28[3):216-234 | #Levy M., Zylber-Katz E., Rosenkranz B., Clinical Pharmacokinetics of Dipyrone and its Metabolites, Clinical Pharmacokinetics. March 1995; 28[3):216-234 | ||
#Schmidt-Hansen M, Bennett Ml, Arnold S, Bromham N, Hilgart JS., Oxycodone for cancer-related pain. ,Cochrane Database of Systematic Reviews 2017, Issue 8 | #Schmidt-Hansen M, Bennett Ml, Arnold S, Bromham N, Hilgart JS., Oxycodone for cancer-related pain. ,Cochrane Database of Systematic Reviews 2017, Issue 8 | ||
| + | #Wiffen PJ, Wee B, Moore RA., Oral morphine for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 4 | ||
| + | #M. Fa I Io n1, R. Giusti2, F. Aie 1113, P. H 0skin4, R. Rol ke 5, M. Sharma6 & C. I. Ripamo nti7, on behalf of the ESMO Guidelines Committee, Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Annals of Oncology 29 [Supplement 4): iv149-iv174,2018 | ||
| + | #Straube C, Derry S, Jackson KG, Wiffen PJ, Bell RF, Strassels S, Straube S. Codeine, alone and with paracetamol [acetaminophen), for cancer pain.Cochrane Database of Systematic Reviews 2014, Issue 9 | ||
| + | #Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT. Results of a Double- Blind, Randomized, Placebo-Controlled Study of Nabiximols Oromucosal Spray as an Adjunctive Therapy in Advanced Cancer Patients with Chronic Uncontrolled Pain, J Pain Symptom Manage. [Feb 2018): 55[2): 179-88 | ||
| + | #Nicholson AB, Watson GR, Derry S, Wiffen PJ. Methadone for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 2 | ||
| + | #Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain. Cochrane Database of Systematic Reviews 2013, Issue 10 | ||
| + | #Corli 0, Floriani I, Roberto A, Montanari M, Galli F, Greco MT, Caraceni A, Kaasa S, Dragani TA, Azzarello G, Luzzani M, Cavanna L, Bandieri E, Gamucci T, Lipari G, Di Gregorio R, Valenti D, Reale C, Pavesi L, lorno V, Crispin0 C, Pacchioni M, ApoIone G; CERP STUDY OF PAIN GROUP: Are strong opioids equally effective and safe in the treatment of chronic cancer pain? A multicenter randomized phase IV 'real life' trial on the variability of response to opioids. Ann Oncol. [Jun 2016); 27[6): 1107-15 | ||
| + | #Jandhyala R, Fullarton JR & Bennett ML Efficacy of Rapid-Onset Oral Fentanyl Formulations vs. Oral Morphine for Cancer- Related Breakthrough Pain: A Meta-Analysis of Comparative Trials. J Pain Symptom Management 2013 Oct; | ||
| + | 46 [4): 573-80 | ||
| + | #Mitchell A, McCrea R Inglis K, Porter G. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine [Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012 Nov; 19[12):3792-800 | ||
| + | |||
| + | </div> | ||
==NEUROPATHIC PAIN / פרופ' עידו וולף== | ==NEUROPATHIC PAIN / פרופ' עידו וולף== | ||
גרסה מ־14:37, 18 בנובמבר 2021
ערך זה נמצא בבדיקה ועריכה על ידי מערכת ויקירפואה, וייתכן כי הוא לא ערוך ומוגה.
|
| |
|---|---|
| אמנות הטיפול התרופתי בכאב בחולה האונקולוגי המבוגר - Pharmacological pain treatment in adults oncology | |
| תחום | רפואה פליאטיבית, פרמקולוגיה קלינית |

| |
| האיגוד המפרסם | איגודים משתתפים |
| קישור | באתר הר"י |
| תאריך פרסום | 2019 |
| יוצר הערך | העורכים |
| ניירות עמדה מתפרסמים ככלי עזר לרופא/ה ואינם באים במקום שיקול דעתו/ה בכל מצב נתון. כל הכתוב בלשון זכר מתייחס לשני המגדרים. | |
לערכים נוספים הקשורים לנושא זה, ראו את דף הפירושים – כאב במחלות ממאירות
LEVELS OF EVIDENCE & GRADES OF RECOMMENDATION
(Adapted from the Infectious Diseases Society of America-United States Public Health Service Grading System)
LEVELS OF EVIDENCE (LOE)
- I - Evidence from at least one large randomised, controlled trial of good methodological quality (low potential for bias) or meta-analyses of well-conducted randomised trials without heterogeneity
II - Small randomised trials or large randomised trials with a suspicion of bias (lower methodological quality) or meta-analyses of* such trials or of trials demonstrated heterogeneity
- III - Prospective cohort studies
- IV - Retrospective cohort studies or case-control studies
- V - Studies without control group, case reports, expert opinions
GRADES OF RECOMMENDATION (GOR)
- A - Strong evidence for efficacy with a substantial clinical benefit, strongly recommended
- B - Strong or moderate evidence for efficacy but with a limited clinical benefit, generally recommended
C - Insufficient evidence for efficacy or benefit does not outweigh the risk or the disadvantages (adverse events, costs, . . .),* optional
- D - Moderate evidence against efficacy or for adverse outcome, generally not recommended
- E - Strong evidence against efficacy or for adverse outcome, never recommended
מקור:
(*) Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149–iv174.
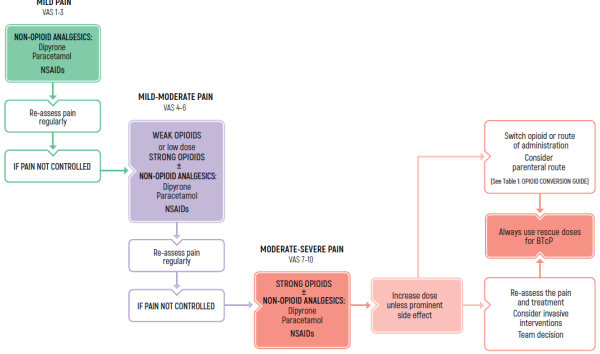
CHRONIC PAIN / ד"ר אורה רוזנגרטן
TREATMENT OF CHRONIC PAIN
- Use around the clock-long acting medications
- Allow rescue medications
- BTcP - breakthrough cancer pain
- NSAIDs - nonsteroidal anti-inflammatory drugs
(*) Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149–iv174.
ADULTS / Chronic Cancer Pain
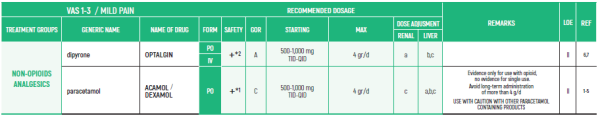
NON-OPIOIDS ANALGESICS:
- PARACETAMOL: Avoid long-term administration of more than 4 g/d. Avoid when patient is ingesting limited food or consumes long-term ethanol.
- DIPYRONE/MITAMIZOLE: Agranulocytosis has been described with varying relative risks in different populations. Patients should be advised to seek for medical care if signs of infection.
- BUC - buccal formulation
- GOR - grades of recommendation
- IR - immediately release
- IV - intravenous formulation
- LOE - levels of evidence
- MCR - morphine controlled release
- MIR - morphine immediate release
- NAS - nasal formulation
- OM - oral mucosal
- PCA - patient controlled analgesia
- PO - per oral formulation
- SC - subcutaneous
- SL - soluble (liquid) concentrate
- SmPC - summary of product characteristics
- SR - slow release
- TDDS - transdermal drug delivery systems
- Q - application
- QD - 1 (once)a day
- BID - 2 (two) times daily
- TID - 3 (three) times daily
- QID - 4 (four) times daily
- PRN - as needed
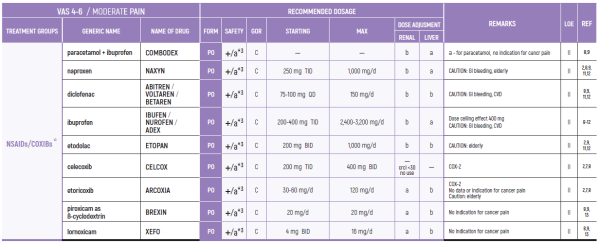
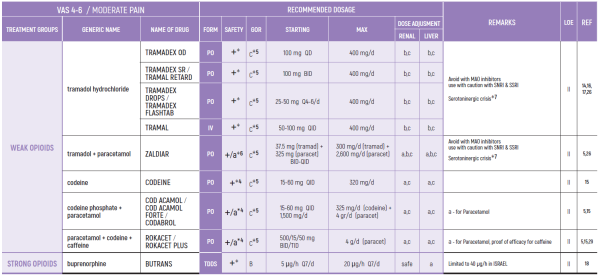
ADULTS / Chronic Cancer Pain
LIMITED USE FOR SHORT PERIODS ONLY RESPONDING PATIENTS: RE EVALUATE FOR LONG TERM USE RISK FACTORS.
NSAIDs:
3. Prolonged use not advised due to concern of side effects such as hypertension, edema, CVD, GI bleeding, renal toxicity and bleeding diathesis weak opioids (8)
WEAK OPIOIDS:
2. Ceiling effect may reduce efficacy and induce side effects (26).
3. Compared to low dose strong opioids - better and faster effect by strong opioids (14).
4. Use with caution with other paracetamol containing products.
5. Tramadol may cause serotoninergic crisis, mostly in elderly, olthough uncommon (26).
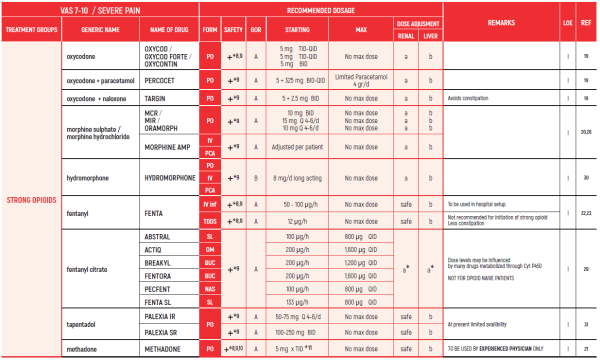
STRONG OPIOIDS:
6. Beware in elderly - may develop confusion.
7. Discontinuation should be gradual to avoid withdrawal symptoms.
10. Methadone is equivalent to morphine in terms of efficacy but needs careful titration. Half-life may differ between people - careful titration needed. Advised to be used by experts only.
11. Methadone starting dose depends on dose of opioid used previously. Equivalence doses of methadone differ at low and high doses of morphine.
CANABIS:
SATIVEX is indicated as adjunctive treatment for the symptomatic relief of neuropathic pain in multiple sclerosis in adults.
SATIVEX may be useful as adjunctive analgesic treatment in adult patients with advanced cancer who experience moderate to severe pain during the highest tolerated dose of strong opioid therapy for persistent background pain.
The indications in the Ministry of Health’s “Procedure 106” are:
2.3.0.0. For patients during treatment with chemotherapy and up to six months after its completion to relieve nausea, vomiting, or pain related to treatment (even without exhaustion of conventional treatments for relief of nausea, etc.). In cases where the attending physician believes cannabis treatment should be continued after half a year- he will specify the reasons for the continuation of the treatment and for what period he believes the treatment should be continued.
22.3.0.3 To relieve pain from a cancerous source at the metastatic stage and after exhausting conventional treatment options.
- ביבליוגרפיה
- Leslie A. Shimp, Pharm.D., Safety Issues in the Pharmacologic Management of Chronic Pain in the Elderly. Pharmacotherapy 1998; 18[6):1313-22
- https://www.drugs.com/dosage
- Cooper TE, Fisher E, Anderson B, Wilkinson NMR, Williams DG, Eccleston C, Paracetamol [acetaminophen) for chronic non-cancer pain in children and adolescents [Review), Cochrane Database of Systematic Reviews 2017, Issue 8. Art. No.: CD012539
- Wiffen PJ, Derry S, Moore RA, McNicol ED, Bell RF, Carr DB, McIntyre M, Wee B. Oral paracetamol [acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 7. Art. No.: CD012637
- Israel JF, Parker G. Llack of benefit from paracetamol in palliative cancer patients reguiriing high doses of opioids: a randomised double blind placebo controlled trial, J Pain and Symptom Management, March 2010; 39[3)
- Gaertner J, Stamer UM, Remi C, Voltz R, Bausewein C. Metamizole/dipyrone for the relief of cancer pain: A systematic review and evidence-based recommendations for clinical practice. Palliat Med. 2017 Jan; 31 [1): 26-34
- Levy M, Zylber-Katz E, Rosenkranz B. Clinical Pharmacokinetics of Dipyrone and its Metabolites, Clinical Pharmacokinetics. March 1995; 28[ 3): 216-234
- Mercandante S, Giarratano A. The long and winding road of non steroidal antinflammatory drugs and paracetamol in cancer pain management: A critical review Critical Reviews in Oncology/Hematology, August 2013; 87[2): 140-5
- Derry S, Wiffen PJ, Moore RA, McNicol ED, Bell RF, Carr DB, McIntyre M, Wee B. Oral nonsteroidal anti-inflammatory drugs [NSAIDs) for cancer pain in adults. Cochrane Database of Systematic Reviews 2017, Issue 7.
- Moore RA, Derry S, Wiffen PJ, Straube S, Aldington DJ. Overview review: Comparative efficacy of oral ibuprofen and paracetamol [acetaminophen) across acute and chronic pain conditions. Eur J Pain [2015);19:1213-23
- Ventafridda V, De Conno F, Panerai AE, Maresca V, Monza GC, Ripamonti C. Non-steroidal anti-inflammatory drugs as the first step in cancer pain therapy: double-blind, within-patient study comparing nine drugs.J Int Med Res. [Jan-Feb 1990); 18[1): 21-9
- Ewan D McNicol Scott Strassel sLeonidas Goudas Joseph Lau Daniel B Carr: NSAIDS or paracetamol, alone or combined with opioids, for cancer pain, Cochrane Systematic Review: 20 April 2005
- Yalcin S, Altundag K, Asil M, Tekuseman G. Sublingual Piroxicam for cancer pain . Med Oncol [Jul 1998); 15[2): 137-9
- Bandieri E, Romero M, Ripamonti Cl, Artioli F, Sichetti D, Fanizza C, Santini D, Cavanna L, Melotti B, Conte PF, Roila F, Cascinu S, Bruera E, Tognoni G, Luppi M. Randomized Trial of Low-Dose Morphine Versus Weak Opioids in Moderate Cancer Pain. J Clin Oncol. [Feb 2016) 10; 34[5): 436-42
- Straube C, Derry S, Jackson KO, Wiffen PJ, Bell RF, Strassels S, Straube S. Codeine, alone and with paracetamol [acetaminophen), for cancer pain.Cochrane Database of Systematic Reviews 2014, Issue 9.
- Eisenberg E, Berkey CS, Carr DB, Mosteller F, Chalmers TC. Efficacy and safety of nonsteroidal antiinflammatory drugs for cancer pain: a meta-analysis. J Clin Oncol. [Dec 1994); 12[12): 2756-65
- Wiffen PJ, Derry S, Moore RA. ramadol with or without paracetamol [acetaminophen) for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 5
- Schmidt-Hansen M, Bromham N, Taubert M, Arnold S, Hilgart JSSchmidt-Hansen M, Bromham N, Taubert M, Arnold S, Hilgart JS. Buprenorphine for treating cancer pain .Cochrane Database of Systematic Reviews 2015, Issue 3
- Schmidt-Hansen M, Bennett Ml, Arnold S, Bromham N, Hilgart JS., Oxycodone for cancer-related pain. ,Cochrane Database of Systematic Reviews 2017, Issue 8.
- Wiffen PJ, Wee B, Moore RA., Oral morphine for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 4.
- Nicholson AB, Watson GR, Derry S, Wiffen PJ. Methadone for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 2
- Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain. Cochrane Database of Systematic Reviews 2013, Issue 10
- Corli 0, Floriani I, Roberto A, Montanari M, Galli F, Greco MT, Caraceni A, Kaasa S, Dragani TA, Azzarell0 G, Luzzani M, Cavanna L, Bandieri E, Gamucci T, Lipari G, Di Gregorio R, Valenti D, Reale C, Pavesi L, lorno V, Crispino C, Pacchioni M, ApoIone G; CERP STUDY OF PAIN GROUP: Are strong opioids egually effective and safe in the treatment of chronic cancer pain? A multicenter randomized phase IV 'real life' trial on the variability of response to opioids. Ann Oncol. [Jun 2016); 27(6): 1107-15
- Sande TA, Laird BJ, Fallon MT, The use of opioids in cancer patients with renal impairment-a systematic review, Support Care Cancer. [Feb 2017); 25[2): 661-75
- King S, Forbes K, Hanks GW, Ferro GJ, Chambers EJ. A systematic review of the use of opioid medication for those with moderate to severe cancer pain and renal impairment: a European Palliative Care Research Collaborative opioid guidelines project. Palliat Med.[Jul 2011); 25[5): 525-52
- Fallon M, Giusti R, Aie 11 i F, Hoskin R Rolke R, Sharma M, Ripamonti Cl; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol [2018);29 [Suppl 4): iv149-iv174.
- Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT. Results of a Double- Blind, Randomized, Placebo-Controlled Study of Nabiximols Oromucosal Spray as an Adjunctive Therapy in Advanced Cancer Patients with Chronic Uncontrolled Pain, J Pain Symptom Manage. [Feb 2018): 55[2): 179-88
- Jandhyala R, Fullarton JR & Bennett Ml. Efficacy of Rapid-Onset Oral Fentanyl Formulations vs. Oral Morphine for Cancer- Related Breakthrough Pain: A Meta-Analysis of Comparative Trials. J Pain Symptom Management 2013 Oct; 46 [4): 573-80
- Mitchell A, McCrea P, Inglis K, Porter G. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine [Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012 Nov; 19[12):3792-800
- Bao YJ, Hou W, Kong XY, Yang L, Xia J, Hua BJ, Knaggs R. Hydromorphone for cancer pain. Cochrane Database Syst Rev. 2016 Oct 11;10
- Mercadante S. Opioid titration in cancer pain: a critical review. Eur J Pain. 2007 Nov;11[8):823-30
- Fallon MT, Albert Lux E, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Lichtman AH & Kornyeyeva E. Sativex oromucosal spray as adjunctive therapy in advanced cancer patients with chronic pain unalleviated by optimized opioid therapy: two double-blind, randomized, placebo-controlled phase 3 studies. Br J Pain. 2017 Aug;11[3):119-133
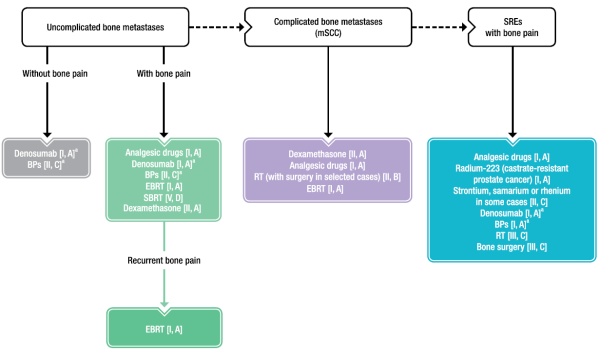
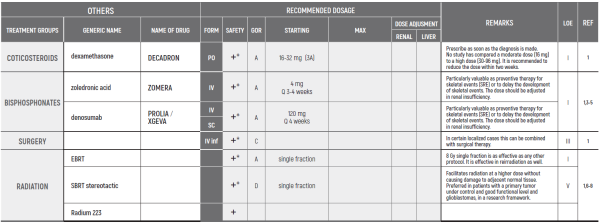
BONE PAIN & SPINAL CORD COMPRESSION / פרופ' פסח שוורצמן
- BTcP - breakthrough cancer pain;
- NSAIDs - nonsteroidal anti-inflammatory drugs
- BP - biphosphonate;
- EBRT - external beam radiotherapy;
- HFRT - hypofractionated radiotherapy;
- mSCC - metastatic spinal cord compression;
- RT - radiotherapy;
- SBRT - stereotactic body radiotherapy;
- SRE - skeletal-related event
Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti CI; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol (2018);29 (Suppl 4): iv149–iv174.
a Do not switch between weak opioids
Remarks:
- NON-OPIOID ANALGESICS - See CHRONIC PAIN
- NSAIDS / COXIBs - See CHRONIC PAIN
- WEAK OPIOIDS - See CHRONIC PAIN
- STRONG OPIOIDS - See CHRONIC PAIN
- CANABIS - See CHRONIC PAIN
ALL OF THESE DRUGS ARE USED WHEN SKELETAL PAIN OR MSCC PAIN IS ACCOMPANIED BY AN ELEMENT OF NEUROPATHIC PAIN.
Comments:
- Most of the studies are Level 2 and not as cited in the ESMO paper.
- The maximal dosage is the one that results in optimal pain relief with minimal adverse effects.
- ביבליוגרפיה
- Fallon M, Giusti R, Aielli F, Hoskin P, Rolke R, Sharma M, Ripamonti Cl; ESMO Guidelines Committee. Management of cancer pain in adults in patients: ESMO clinical practice guidelines. Ann Oncol [2018);29 [Suppl 4): iv149-iv174.
- Wiffen PJ, Wee B, Derry S, Bell RF, Moore RA. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7:CD012592
- Schmidt-hansen M, Bromham N, Taubert M, Arnold S, Hilgart JS. Buprenorphine for treating cancer pain. Cochrane Database Syst Rev. 2015;[3]:CD009596
- Kane CM, Hoskin R Bennett Ml. Cancer induced bone pain. BMJ. 2015:350:11315־
- Von moos R, Body JJ, Egerdie B, et al. Pain and analgesic use associated with skeletal-related events in patients with advanced cancer and bone metastases. Support Care Cancer. 2016;24[3):1327-37.
- Tsuzuki S, Park SH, Eber MR, Peters CM, Shiozawa Y. Skeletal complications in cancer patients with bone metastases. Int J Urol. 2016;23[10):825-832
- De felice F, Piccioli A, Musio D, Tombolini V. The role of radiation therapy in bone metastases management. Oncotarget. 2017;8[15):25691-25699
- Ejima Y, Matsuo Y, Sasaki R. The current status and future of radiotherapy for spinal bone metastases. J Orthop Sci. 2015;20[4):585-92
- Israel JF, Parker G, Llack of benefit from paracetamol in palliative cancer patients reguiriing high doses of opioids: a randomised double blind placebo controlled trial, J Pain and Symptom Management, March 2010; 39[3]
- Gaertner JI, Stamer UM2, Remi C3, Voltz R4, Bausewein C3, Metamizole/dipyrone for the relief of cancer pain: A systematic review and evidence-based recommendations for clinical practice. Palliat Med. 2017 Jan; 31[1):26-34
- Levy M., Zylber-Katz E., Rosenkranz B., Clinical Pharmacokinetics of Dipyrone and its Metabolites, Clinical Pharmacokinetics. March 1995; 28[3):216-234
- Schmidt-Hansen M, Bennett Ml, Arnold S, Bromham N, Hilgart JS., Oxycodone for cancer-related pain. ,Cochrane Database of Systematic Reviews 2017, Issue 8
- Wiffen PJ, Wee B, Moore RA., Oral morphine for cancer pain. Cochrane Database of Systematic Reviews 2016, Issue 4
- M. Fa I Io n1, R. Giusti2, F. Aie 1113, P. H 0skin4, R. Rol ke 5, M. Sharma6 & C. I. Ripamo nti7, on behalf of the ESMO Guidelines Committee, Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Annals of Oncology 29 [Supplement 4): iv149-iv174,2018
- Straube C, Derry S, Jackson KG, Wiffen PJ, Bell RF, Strassels S, Straube S. Codeine, alone and with paracetamol [acetaminophen), for cancer pain.Cochrane Database of Systematic Reviews 2014, Issue 9
- Lichtman AH, Lux EA, McQuade R, Rossetti S, Sanchez R, Sun W, Wright S, Kornyeyeva E, Fallon MT. Results of a Double- Blind, Randomized, Placebo-Controlled Study of Nabiximols Oromucosal Spray as an Adjunctive Therapy in Advanced Cancer Patients with Chronic Uncontrolled Pain, J Pain Symptom Manage. [Feb 2018): 55[2): 179-88
- Nicholson AB, Watson GR, Derry S, Wiffen PJ. Methadone for cancer pain. Cochrane Database of Systematic Reviews 2017, Issue 2
- Hadley G, Derry S, Moore RA, Wiffen PJ. Transdermal fentanyl for cancer pain. Cochrane Database of Systematic Reviews 2013, Issue 10
- Corli 0, Floriani I, Roberto A, Montanari M, Galli F, Greco MT, Caraceni A, Kaasa S, Dragani TA, Azzarello G, Luzzani M, Cavanna L, Bandieri E, Gamucci T, Lipari G, Di Gregorio R, Valenti D, Reale C, Pavesi L, lorno V, Crispin0 C, Pacchioni M, ApoIone G; CERP STUDY OF PAIN GROUP: Are strong opioids equally effective and safe in the treatment of chronic cancer pain? A multicenter randomized phase IV 'real life' trial on the variability of response to opioids. Ann Oncol. [Jun 2016); 27[6): 1107-15
- Jandhyala R, Fullarton JR & Bennett ML Efficacy of Rapid-Onset Oral Fentanyl Formulations vs. Oral Morphine for Cancer- Related Breakthrough Pain: A Meta-Analysis of Comparative Trials. J Pain Symptom Management 2013 Oct;
46 [4): 573-80
- Mitchell A, McCrea R Inglis K, Porter G. A randomized, controlled trial comparing acetaminophen plus ibuprofen versus acetaminophen plus codeine plus caffeine [Tylenol 3) after outpatient breast surgery. Ann Surg Oncol. 2012 Nov; 19[12):3792-800
NEUROPATHIC PAIN / פרופ' עידו וולף
BREAKTHROUGH PAIN / ד"ר דניאלה זלמן
OPIOID - REFRACTORY & RESISTANT PAIN / ד"ר איריס גלוק, ד"ר אופיר מורג, ד"ר יקיר רוטנברג
איגודים משתתפים
- אגודה ישראלית לכאב
- האיגוד הישראלי לאונקולוגיה קלינית ורדיותרפיה
- האיגוד הישראלי להמטולוגיה ואונקולוגיה ילדים
- האיגוד לרפואה פליאטיבית בישראל
- האיגוד הישראלי לרפואה פנימית
- החוג לטיפול בכאב של איגוד רופאי המשפחה
- איגוד הכירורגים בישראל
- האיגוד הישראלי לאורתופדיה
- האיגוד הישראלי לפרמקולוגיה קלינית - רפואה, ייעוץ ומחקר בתרופות
העורכים
- פרופ' אליעד דוידסון - יו"ר האגודה הישראלית לכאב, מנהל היחידה לשיכוך כאב, המרכז הרפואי הדסה עין-כרם
- ד"ר וילמוש מרמרשטיין - יו"ר האיגוד הישראלי לאונקולוגיה קלינית ורדיותרפיה
- ד"ר יקיר רוטנברג - יו"ר האיגוד הפליאטיבי באיגוד הישראלי לאונקולוגיה קלינית ורדיותרפיה, מח׳ אונקולוגית, המרכז הרפואי הדסה עין-כרם
- פרופ' פסח שוורצמן - יו"ר האיגוד הישראלי לרפואה פליאטיבית, מנהל יחידה פליאטיבית, המרכז הרפואי האוניברסיטאי סורוקה
- פרופ' עידו וולף - מנהל המערך האונקולוגי, המרכז הרפואי ת"א
- ד"ר אורה רוזנגרטן - מנהלת היח׳ לאונקולוגיה גניקולוגית, המרכז הרפואי שערי צדק
- ד"ר דניאלה זלמן - רופאה בכירה, אחראית מחלקת אשפוז רדיותרפיה, המערך האונקולוגי, המרכז הרפואי רמב"ם
- ד"ר איריס גלוק - מנהלת המערך לטיפול תומך, מומחית באונקולוגיה ובטיפול תומך, המרכז הרפואי ע"ש חיים שיבא, תה"ש
- ד"ר אופיר מורג - מנהלת מרפאת כאב אונקולוגי, מומחית ברפואת שיכוך כאב ואונקולוגיה רפואית, המרכז הרפואי ע"ש חיים שיבא, תה"ש
- ד"ר סילביו בריל - מנהל המכון לשיכוך כאב, המרכז הרפואי ת"א
- ד"ר איתי גור-אריה - מנהל המכון לשיכוך כאב, המרכז הרפואי ע"ש חיים שיבא, תה"ש
- פרופ' אילון איזנברג - מנהל היחידה לחקר הכאב, המרכז הרפואי רמב"ם
- פרופ' משה סלעי - מנהל החטיבה האורתופדית, המרכז הרפואי ת"א
- פרופ' אבישי אליס - יו"ר האיגוד הישראלי לרפואה פנימית, מנהל מח׳ פנימית ג', המרכז הרפואי רבין, ביה"ח בילינסון
- פרופ' גיל בר-סלע - מנהל המרכז למחלות סרטן, מרכז רפואי העמק
- ד"ר מיכל שני - יו"ר האיגוד הישראלי לרפואת משפחה
- ד"ר ורד סימוביץ - יו"ר החוג לטיפול בכאב, איגוד רופאי המשפחה בישראל, מומחית ברפואת משפחה, מנהלת רפואית של חטיבת התפעול, מכבי שירותי בריאות


 כניסה
כניסה  עקבו אחרינו בפייסבוק
עקבו אחרינו בפייסבוק